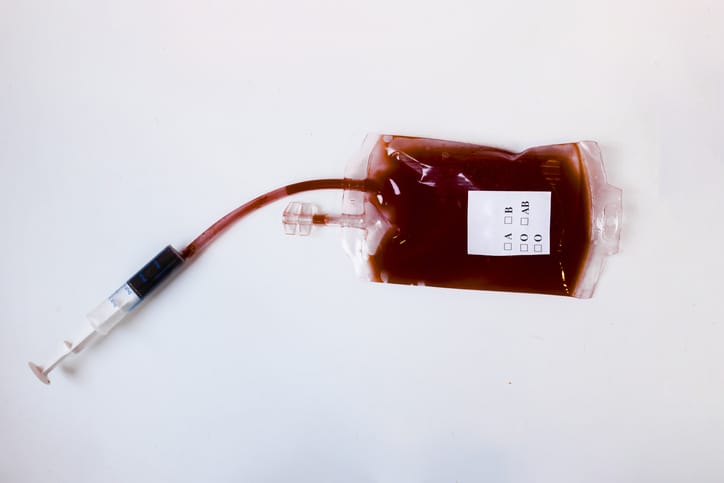
Blood transfusions are an essential part of treatment for hemolytic disease of the fetus and newborn (HDFN).
As maternal antibodies attack and destroy the baby’s red blood cells, this causes anemia and can lead to life-threatening complications. The process of washing red blood cells received from donors removes plasma and other substances, making them safe for transfusion and reducing the risk of complications.
What is HDFN?
Hemolytic disease of the fetus and newborn (HDFN) is an immune-mediated red blood cell disorder that occurs when a baby’s RBCs break down quickly, which is called hemolysis. HDFN is caused by a mismatch between a mother’s and her baby’s blood type (A, B, AB, or O) or Rhesus (Rh) factor (Rh-positive or Rh-negative) during pregnancy.
Why do red blood cells need to be washed?
In HDFN, blood transfusions replace destroyed red blood cells during pregnancy and post-delivery. The donated red blood cells are matched to the baby’s blood type and lack the antigen the maternal antibodies are attacking. To reduce the risk of allergic reactions or other side effects, plasma, antibodies, and other substances are removed by washing before transfusion. This leaves only pure red blood cells.
Red blood cells are not always washed before infusion in HDFN in intravenous transfusions. However, their use is standard practice in the case of exchange transfusions in newborns and in high-risk infants, such as preterm or critically ill babies.
What is the procedure to wash red blood cells?
The procedure of washing red blood cells is performed by using a centrifuge and a sterile saline solution. Around 10% to 20% of red blood cells are lost in the process, so a larger volume of blood is required than in a typical transfusion.
Administering washed red blood cells
Intrauterine blood transfusions are performed during pregnancy when the fetus is diagnosed with HDFN-related anemia. It reduces the risk of severe anemia occurring as it boosts the fetus’s red blood cell count. The washed red blood cells selected from a blood donor bank are infused into the fetus via a long thin needle inserted into the mother’s abdomen that the passes into the umbilical cord or the fetus’s abdomen. Intrauterine blood transfusions are usually required every few weeks until birth to ensure the best fetal outcomes.
In newborns, blood transfusions are required in cases of severe anemia. In some serious cases, exchange transfusions remove part of the baby’s blood and replace it with the donor blood. This helps resolve jaundice as well as anemia as it lowers bilirubin levels and removes residual maternal antibodies in the baby’s blood.
Sign up here to get the latest news, perspectives, and information about HDFN sent directly to your inbox. Registration is free and only takes a minute.